A semen analysis is a routine male fertility investigation and can be requested by your GP or a specialist. It is essential that all couples looking to conceive using partner sperm have a semen analysis.
The semen analysis test aims to assess the three fundamental aspects of sperm function and quality, as described by the World Health Organization. These are:
Sperm concentration
This is also known as the sperm count, and it’s measured in millions of sperm per millilitre of semen (M/ml). Increasing sperm concentration and the total sperm number (the sperm concentration multiplied by semen volume in mls) are both correlated to the chance of pregnancy, whether natural or in fertility treatment. We are ideally looking for a sperm concentration above 15M/ml.
Sperm motility
Sperm motility is the ability of the sperm to swim, and it’s the most important function that we assess. We are looking for at least 32% of sperm to be swimming in a forward direction.
At NUH Life we use computer-assisted semen analysis (CASA) to measure not just how many sperm are swimming, but how fast they are swimming.
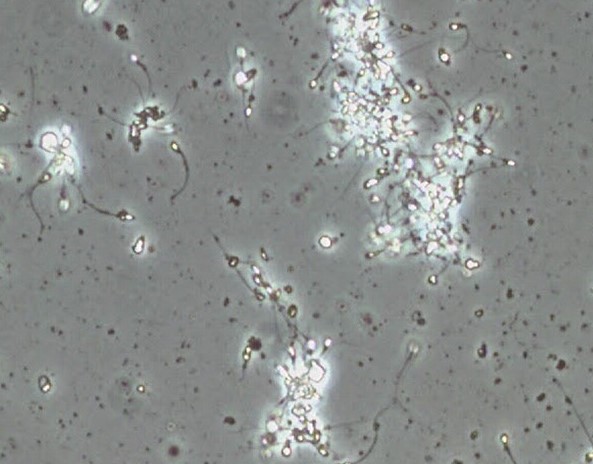
The computer takes a short 1-second video of sperm, and use this to assess both sperm concentration (sperm number) and motility at the same time. The major advantage that CASA has over manual methods, is that for any given test or sample, the lab will get the same results, no matter which member of staff performs it.

Video generated by CASA. Sperm are tracked for 1 second to give individual sperm swimming speeds. By limiting the field to only a second we minimise ‘over-estimation’ of the motile sperm fraction as they leave and enter the area whilst being examined down the microscope. Only those sperm that can be followed for the full 1 second are assessed.

Sperm morphology
Sperm morphology is the shape of the sperm. We’re looking for at least 4% of sperm to have the perfect tadpole shape, with no lumps or bumps.
Morphology is the most controversial sperm parameter assessed, as it is very subjective and open to interpretation. The most recent scientific evidence from large studies in IVF suggest that the % of what we perceive as ‘normal sperm’ does not predict whether your treatment will be successful or not.
However this does not mean that sperm morphology is unimportant, as we know that sperm of certain shape, size and structure are incapable of reaching and fertilising the egg. (For example, the 3-headed sperm pictured here).
Other measures
Ejaculate volume: Measured in millilitres, a normal volume is around 1.5mls (under half a teaspoon).
Having a normal volume shows us that the glands, such as the prostate and seminal vesicles, are working properly. A very low volume or no fluid at all (0.5ml) can indicate that the semen is going into the bladder instead (known as retrograde ejaculation).
pH: Semen pH should be slightly alkaline (usually between 7.2-8.3). A low pH with an absence of sperm can indicate a blockage or obstruction – known as obstructive azoospermia.
Agglutination and aggregation: The importance of this is often under-estimated. Live sperm can stick to each other which stops them from swimming. Not only is this an indicator for infertility, but this problem can worsen with time.
It also means that estimating sperm number and motility is very difficult and often inaccurate, because all of our methods rely on us having the sperm evenly spread throughout the sample.
Other sperm tests
Anti-sperm antibodies
Antibodies to a man’s sperm have been suggested to be a cause of infertility for many years. They are strongly linked with reduced motility (swimming ability) and agglutination (see above), but there is no evidence other than this that antibodies are produced which may block fertilisation.
Since both poor motility and agglutination are evident from the semen analysis without further testing, the testing for anti-sperm antibodies is not routinely performed.
DNA fragmentation and Reactive oxygen species
High levels of DNA fragmentation (DNA damage) have been associated with poorer sperm quality and, according to some studies, reduced chance of conception. However the strongest published evidence links sperm DNA damage to a higher chance of miscarriage. There are several different types of DNA fragmentation test, but no agreement amongst professionals as to which gives the most reliable results. Any test of DNA fragmentation is unlikely to affect the management of a couple’s infertility or choice of treatment. This is why it’s not routinely offered by the NHS, nor is it part of standard guidance from the WHO.
The same is true for reactive oxygen species (ROS). Although ROS are implicated in a number of disease processes, there is no way to say that the ROS levels in semen are so high that you cannot achieve a pregnancy. In addition, samples with both high levels of DNA damage and ROS usually have other more obvious problems, such as low sperm count, motility or poor morphology.
Male factor infertility – interpreting semen analysis
The assessment of male infertility is not a precise science – quite often the answer is not black and white, but a huge grey area, and also needs to be taken in the context of the female partner.
Male factor infertility can therefore range from something quite severe and well-defined (such as there being no sperm present – azoospermia) to something almost insignificant, like one of the semen parameters being slightly low.
Two thirds of men who attend clinic will have sperm characteristics (sperm parameters) in the ‘normal’ reference range, as defined by the World Health Organisation (WHO).
World Health Organisation normal reference values for describing semen analysis:
| Semen parameter | “Normal” reference value | Term if low |
| Ejaculate volume | 1.5mls | |
| Sperm concentration | 15 million/ml | Oligozoospermia (low)/ Azoospermia (no sperm) |
| Sperm motility | 32% progressive | Asthenozoospermia |
| Sperm morphology | 4% normal forms | Teratozoospermia |
It’s important to remember:
- Just because a male has one or two of these ‘semen parameters’ outside of the normal range, it does not mean that the sample cannot still overall be normal. Some of these values are percentages – therefore if the sperm count is 100 million instead of 15 but the sperm motility is only 10%, the count will more than compensate. Likewise, the count could be only 10 million, but the motility could be 75%.
- Just because a sample is outside of the normal range, it does not mean that the male cannot father a child. It just suggests that his chances are lower.
- If a male’s first sample is deemed abnormal, it does not mean that the next one will be. It’s important that he follows our instructions for sample collection at the time, as we are looking for trends.
- To put these reference ranges into perspective, if a male has a vasectomy operation to make him sterile and a single motile sperm is seen in his sample after the operation, the operation will be deemed a failure and would need repeating.
